Friedreich’s ataxia overview
Friedreich’s ataxia (FA) is a rare, inherited, and progressive disease that primarily affects the nerves and muscles. Named after the German scientist who first described it, FA is characterized by the hallmark symptom of ataxia — a loss of muscle control and coordination — with other symptoms that include speech difficulties, heart problems, and skeletal abnormalities.
A degenerative nervous system disease, FA is estimated to affect about 1 in 40,000 people worldwide, and in the U.S., about 1 in every 50,000 people. Symptom onset usually occurs in childhood or adolescence, between the ages 5 and 15, but symptoms can develop at older ages.
FA’s progressive nature means that most patients will need a wheelchair within 10 to 20 years of symptom onset. There is no cure for FA, but treatment can help to manage symptoms and slow disease progression.
What is Friedreich’s ataxia?
Ataxias are conditions marked by a loss of muscle control and coordination, and they can arise from a wide range of genetic or nongenetic causes. FA is the most common hereditary cause of ataxia, accounting for about 50% of all ataxia cases, and about three-quarters of those seen in people younger than age 25.
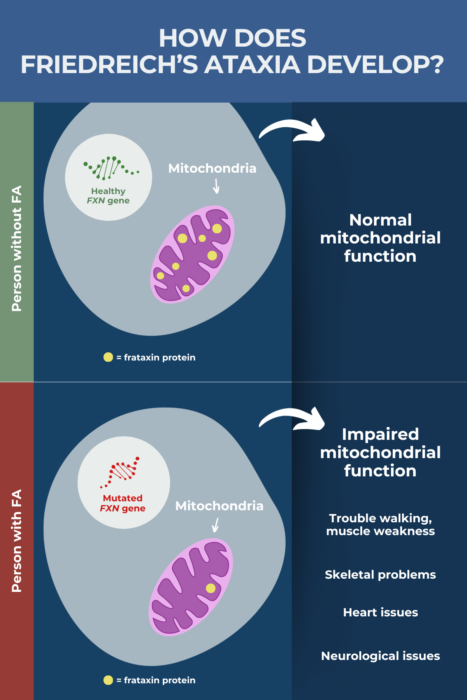
While the symptoms of various ataxias can be similar, FA is distinguished by its underlying mechanisms, leading to low levels of the frataxin protein. Frataxin is important for helping organelles called mitochondria generate cellular energy.
With insufficient frataxin levels, mitochondria are not able to properly power cells. Nerve and muscle cells, which have high energy needs, are particularly vulnerable to the lack of frataxin, leading to nerve damage and movement difficulties for FA patients.
What causes FA?
FA is caused by mutations in the FXN gene, which provides instructions for making the frataxin protein. The most common type of mutation seen in FA is called a GAA trinucleotide repeat expansion, where a trio of DNA nucleotides or building blocks — GAA — is repeated too many times in FXN, disrupting the gene’s ability to produce frataxin. More rarely, another type of FXN mutation is present wherein a single nucleotide is deleted, inserted, or changed.
As a result, not enough frataxin is produced, affecting mitochondria’s ability to produce cellular energy. This leads to nerve cell damage, particularly in areas of the spinal cord that normally are involved in movement control.
Everyone inherits two copies of FXN, one from each biological parent. FA is inherited in an autosomal recessive manner, meaning it develops only where a person carries a mutation in both gene copies. People with one mutated gene copy are considered disease carriers — they will not develop FA symptoms, but they could pass the mutation on to their biological children.
As a genetic disease, the greatest risk factor for FA is inheritance, meaning a family history of the condition. FA most commonly is found in people of European ancestry.
What are the symptoms of FA?
The hallmark symptom of FA — and the one that gives it its name — is ataxia. The first symptoms to become apparent for most patients are gait ataxia (trouble walking) or general clumsiness. Over time, additional motor symptoms, such as profound muscle weakness and balance problems, become evident, and most patients will be wheelchair-reliant within 10 to 20 years after symptoms appear.
Other FA symptoms may include:
- Muscular issues: As FA progresses, ataxia and muscle weakness in the lower limbs can spread to the upper limbs and trunk, leading to speech difficulties that make patients difficult to understand. In advanced disease stages, swallowing difficulties also may arise.
- Skeletal problems: Changes in muscle strength may contribute to bone changes in patients. Scoliosis, an abnormal curvature of the spine, is very common in FA, as are certain bone abnormalities in the feet.
- Heart issues: Cardiac problems are common with FA, and are the leading cause of death among patients. The most common heart condition is hypertrophic cardiomyopathy, where the cardiac muscles that line the heart become thick and enlarged, making it more difficult to pump blood. Abnormal heart rhythms or scar tissue buildup in the heart also can occur.
- Neurological issues: Nerve cell degeneration in FA may cause neurological problems, including abnormal eye movements, some decline in vision or hearing, and sensory impairments like a diminished sense of touch.
- Diabetes: The loss of frataxin may contribute to problems in insulin production or response, leading to elevated blood sugar levels.
- Bladder and bowel issues: Symptoms including urgent and frequent urination, constipation, or incontinence have been described in people with FA, all of which affect quality of life.
- Sexual dysfunction: Some patients report problems that include erectile dysfunction, insufficient vaginal lubrication, or reduced genital sensations.
How is FA diagnosed?
A definitive FA diagnosis can be reached by genetic testing to look for mutations in the FXN gene. That test usually is performed when a doctor suspects the disease, after conducting a comprehensive physical exam and gathering the patient’s medical and family history.
Other tests that can be used to help diagnose FA or rule out other conditions include:
- nerve conduction studies, used to assess nerve damage
- electromyography, a test of nerve and muscle health
- tests of heart structure and function, such as electrocardiography given measures the heart’s electrical rhythms, and echocardiography, which creates an image of the heart to assess muscle thickness and functions like blood flow
- MRI scans can look for signs of nerve degeneration and atrophy in the brain and spinal cord, and also help to distinguish FA from other ataxias or conditions with similar symptoms. Cardiac MRIs may be used to identify heart disease.
- urine or blood tests look for signs of diabetes or are used to rule out other causes of ataxia.
How is FA treated?
Although there is no cure, a number of treatments can help to ease symptoms and slow the progression of FA.
Medications
Skyclarys (omaveloxolone) is the only therapy specifically approved for FA. The medication is indicated for patients ages 16 or older and is taken as oral capsules once each day. It helps to increase cellular energy production, which is expected to slow and possibly stop FA progression.
Other medications can be used to control heart disease and its symptoms, ease spasticity (muscle rigidity), or to lower blood sugar levels in patients with FA-associated diabetes.
Surgery
Scoliosis is a sideways curvature of the spine that can affect posture, cause pain, and make breathing difficult. If this skeletal problem becomes advanced, patients may require corrective surgery.
Likewise, foot deformities can cause discomfort and impede movement for FA patients able to walk. Corrective surgery can help prevent the progression or recurrence of foot problems, allowing patients to maintain physical function longer.
Physical therapy and exercise
Exercise and physical therapy can help in managing some FA symptoms and improve overall fitness, including strengthening and stretching the muscles and aiding coordination and balance. Physical activity also helps with mental health issues such as depression and anxiety, improves sleep, and eases fatigue, among other benefits.
Physical therapy should be given under the supervision of a trained healthcare professional. The type and duration of therapy given will be tailored to a person’s particular needs.
Adaptive equipment and aids
People living with FA may require specialized equipment to go about their daily activities and minimize the risk of falls. Because FA is progressive, patients over time may become increasingly reliant on such equipment.
Adaptive equipment of use to patients could include:
- walkers
- rollators
- wheelchairs
- mobility scooters
- handrails
- stairlifts
- bathroom adaptations
- adaptive clothing
- reaching aids.
Certain technologies, such as smart home electronics with voice-activated controls, also can help FA patients be more independent in daily life.
What is the prognosis of FA?
Life expectancy with FA tends to be shorter than that of the general public. Research estimates that patients on average live into their 40s or 50s, but some patients survive well into their sixth, seventh, or eighth decade of life.
A number of factors can influence an FA prognosis. For example, symptom severity and age at disease onset seem to be associated with the number of GAA repeats in the FXN gene, the cause of FA. In general, more repeats result in more disruption to the gene, and less frataxin being produced. People with more than 300 repeats tend to experience an earlier disease onset and more severe symptoms than those with 300 or fewer repeats.
FA typically emerges in childhood or adolescence, with most patients experiencing their first symptoms before age 25. Still, about a quarter of patients have late-onset (after age 25) or very late-onset disease (after age 40), which is associated with a milder course.
Heart disease is the leading cause of death in FA, and its presence and severity influences a person’s survival. Severe heart disease is less likely in people with late-onset FA.
Appropriate and timely FA treatment, including medications and physical therapy, affect a patient’s prognosis. To date, Skyclarys is the only approved FA-specific therapy. Clinical trial data indicate Skyclarys can slow disease progression, but it remains unknown whether this medication extends life over the long term.
Friedreich’s Ataxia News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- How Friedreich’s ataxia fits into my summer goals
- Nutrition monitoring may help patients keep healthy weight: Study
- Past doctor visits made me feel more like a specimen than a person
- In life with mobility issues, what’s the best that could happen?
- Grassroots events, education help raise Friedreich’s ataxia awareness
Related articles

 Fact-checked by
Fact-checked by