FAQs about Skyclarys
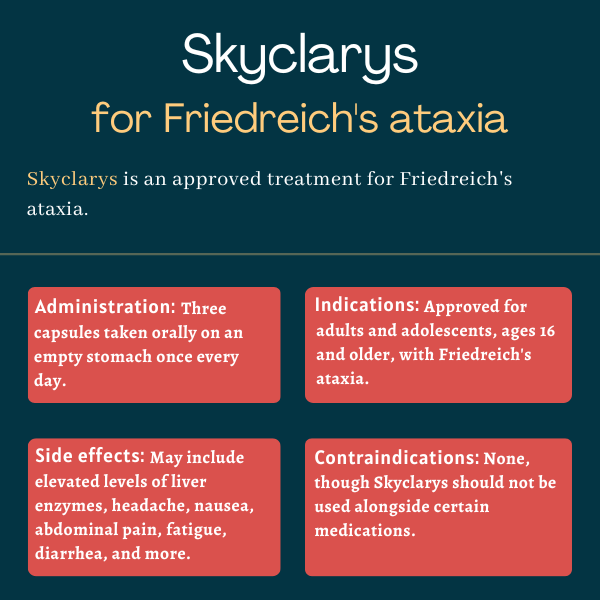
Skyclarys was approved by the U.S. Food and Drug Administration (FDA) in February 2023 for adults and adolescents, ages 16 and older, with Friedreich’s ataxia. The FDA’s approval made Skyclarys the first and only therapy for the disease in the U.S.
Friedreich’s ataxia (FA) is characterized by dysfunction of mitochondria, which are the energy production centers in cells, chronic inflammation, and oxidative stress, a type of cell damage marked by overproduction of toxic reactive oxygen species that outweighs the body’s antioxidant defenses. Skyclarys is intended to activate NrF2, which stands for nuclear factor erythroid 2-related factor 2, a type of protein called a transcription factor whose signaling is impaired in people with FA. NrF2 activates genes that promote mitochondrial function, boost antioxidant responses, and prevent inflammation.
There is no direct evidence reported of an interaction between alcohol and Skyclarys. Patients are, however, advised to talk to their healthcare providers about the use of alcohol or other substances while taking Skyclarys.
In the Phase 2 MOXIe trial (NCT02255435), whose results supported the approval of Skyclarys by the U.S. Food and Drug Administration, improvements in the function of mitochondria (the so-called powerhouses of cells) and in neurological function were most evident about three months (12 weeks) after starting Skyclarys treatment. Benefits were seen as early as four weeks into therapy. There is, however, no standard timeline for Skyclarys’ benefits, as each person may respond differently to the medication.
The most common side effects of Skyclarys are elevated levels of liver enzymes, headache, nausea, abdominal pain, fatigue, diarrhea, and musculoskeletal pain; such pain may affect bones, joints, ligaments, tendons, or muscles. The therapy’s prescribing information includes warnings about the risk of increased liver enzymes, high levels of B-type natriuretic peptide (BNP), which is a marker of heart function, and changes in the blood levels of cholesterol, all of which have happened in clinical testing. Measurements of each of these levels are recommended before and periodically after starting treatment.
Related Articles

 Fact-checked by
Fact-checked by