Symptoms of Friedreich’s ataxia
Friedreich’s ataxia (FA) is a rare condition marked by the hallmark symptom of ataxia, which is characterized by a lack of coordination and muscle control during voluntary movements.
Mutations in the FXN gene lead to a lack of the frataxin protein that’s important for helping produce cellular energy. Nerve and muscle cells — which have high energetic needs — are particularly vulnerable to the loss of frataxin, leading to degeneration of the nerves involved in muscle control and muscle wasting.
While nerve and muscle degeneration are cardinal manifestations of the disease, FA affects many parts of the body, leading to a wide range of other symptoms.
FA symptoms usually emerge between the ages of 5-15 and progressively worsen over time. Nevertheless, FA age of onset and the severity and FA progression varies based on the underlying genetic mutation and other clinical factors. While there is no cure, FA treatments are available to slow disease progression or ease certain symptoms.
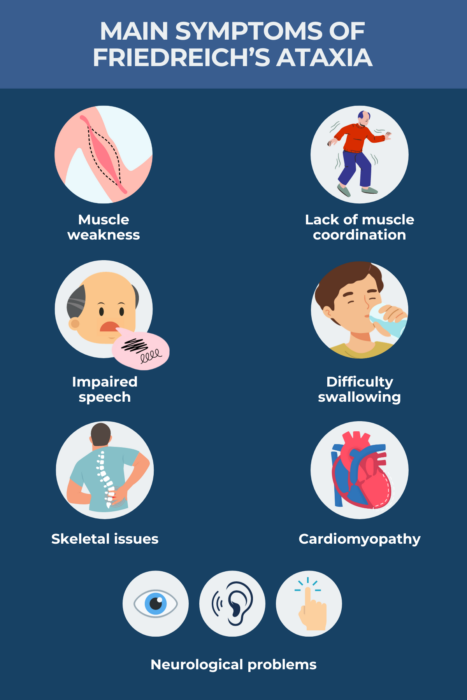
Ataxia and muscle weakness
FA is characterized by progressive degeneration of the nerve fibers running from the body to the spinal cord (peripheral nerves) and of the cerebellum — a brain region that coordinates voluntary movement. As such, sensory inputs from the body to the brain, and commands from the brain back down to the body are impaired.
This leads to ataxia. According to the National Ataxia Foundation, ataxia can look a bit like being intoxicated, with common manifestations including lack of coordination, stumbling, falling, and slurred speech. As the disease progresses, people with FA usually experience profound muscle weakness that significantly impacts walking, upper limb movements, speech, and swallowing.
Limbs
Difficulty walking, or gait ataxia, is typically the first symptom to become apparent in FA. It may first manifest as simply unsteadiness, but patients experience progressive losses in balance and weakness in the leg muscles. A loss of reflexes, particularly in the knees and ankles, also is observed.
Patients usually become increasingly reliant on walking aids to move around. While the rate of FA progression varies, a majority of patients will need a wheelchair within 10-20 years after their symptoms first appear.
Patients who have lost the ability to walk may maintain upper body strength for some time, but ataxia and muscle weakness can eventually progress to affect the arms and trunk. Problems with dexterity and upper limb coordination cause daily life activities to become increasingly challenging.
Some people with FA also may experience spasticity (when muscles are abnormally tight), which can lead to painful muscle spasms.
Speech and swallowing
Because FA also affects the muscles used to coordinate speech, patients commonly experience dysarthria, or difficulty speaking. Early on, this presents as slow, slurred speech, often involving slow, jerky, and hesitant speech patterns. As FA progresses, speech may become almost unintelligible. Speech problems do not reflect impairments in language skills or cognitive abilities.
Weakness in the muscles needed for swallowing is common in later stages, leading to difficulty swallowing, or dysphagia. To avoid food entering the airways, leading to choking or respiratory infections, a modified diet may be required.
Skeletal issues
FA patients commonly experience skeletal abnormalities, which are thought to arise when changes in muscle strength pull the bones into unusual positions.
Scoliosis, an abnormal curvature of the spine, is a common FA symptom that emerges early in the disease course. The reported prevalence of scoliosis varies, but is believed to occur in at least two-thirds of patients. As it progresses, scoliosis can affect posture, cause pain, and impact breathing. It thus often requires corrective surgery.
FA patients may also experience skeletal abnormalities in the feet, including:
- high arches, or pes cavus
- clubfoot, or talipes equinovarus
- toe deformities, or hammer toe
- foot inversions, or feet turning inward.
These foot abnormalities may contribute to gait abnormalities and unsteadiness among FA patients who are still able to walk. These issues may require treatment with braces or surgery.
Cardiomyopathy and other heart problems
Heart abnormalities affect about three-quarters of FA patients to some degree, with heart disease being the leading cause of death in FA. Still, the severity of cardiac abnormalities varies significantly from mild and asymptomatic to life-threatening.
The most common cardiac change observed in FA patients is hypertrophic cardiomyopathy. In the condition, the cardiac muscles lining the heart (ventricular walls) become thick and enlarged, shrinking the heart’s blood-filled chambers and decreasing its capacity to pump blood. Heart muscles adapt to these increased demands by increasing in size, a condition called hypertrophy.
Over time, cardiomyopathy may cause arrhythmias, or irregular heartbeats, that can be life-threatening. Arrhythmias in FA may include tachycardia (fast heart rate) or a slow heart rate accompanied by abnormal electrical signaling in the heart.
Scar tissue also may build up in the FA heart, a condition known as myocardial fibrosis, further contributing to heart function declines.
Not all heart problems will cause overt symptoms, but some signs of cardiac involvement may include:
- extreme fatigue
- chest pain
- shortness of breath, especially with exertion
- abnormally rapid, fluttering or pounding heart (palpitations).
Early on in the disease, cardiac changes may not have a significant effect on the heart’s ability to function. Over time, as damage to the heart accumulates, some patients with cardiac involvement will eventually experience heart failure, when the heart is unable to adequately pump blood through the body. Symptoms include leg swelling, difficulty breathing while lying flat, persistent cough, or extreme fatigue.
While cardiac issues are the leading cause of death in FA, most people who die of heart problems will do so before age 40. Moreover, most people with cardiac-related death will die within 10 years of disease onset, whereas the risk of cardiac-associated death decreases significantly once a person has been living with FA for more than 20 years.
Neurological problems
In addition to problems with muscle control, nerve damage and degeneration in FA may affect the brain, including changes in the way the brain processes visual, auditory, or other sensory inputs.
Visual impairment and hearing loss
Many FA patients exhibit eye-related abnormalities, including abnormal eye movements or damage to the nerves connecting the eyes to the brain (optic neuropathy). However, these changes are often subclinical, meaning they don’t lead to significant vision problems. While some patients experience slow declines in visual acuity over time, substantial visual impairments and blindness are rare.
Likewise, abnormal neurological processing of auditory signals is seen commonly in FA, but significant problems with sound perception or deafness are uncommon.
Sensory impairment
Damage to the peripheral and spinal cord nerves, which are important for sensory perceptions, is associated with sensory loss in FA. A loss of touch (tactile sensations) is very common, but may only be detected in laboratory studies.
Sensations related to vibration and movement/position (proprioception) also may be impaired early on, whereas perceptions of light touch, pain, and temperature can be affected in later disease stages.
Brain atrophy
Atrophy, also known as wasting or shrinkage, of nervous system tissue is common in people with FA and may worsen over time as the disease progresses. This tissue loss can be detected with an MRI scan.
Shrinkage is seen earliest and most significantly in certain areas of the spinal cord, where nerves important for relaying sensory and motor signals between the brain and the rest of the body reside. Thus, spinal cord wasting contributes to other FA symptoms, such as sensory impairments and movement problems. The cervical, or neck region, of the spinal cord is often particularly affected.
Parts of the brain might also exhibit signs of atrophy, although usually to a lesser extent than in the spinal cord. For example, the cerebellum — a region at the back of the brain involved in movement control and balance — may be smaller in some people with FA than in healthy people, but it does not shrink to the same extent as that seen in people with other types of ataxia. Other areas of the brain may be increasingly affected as the disease progresses, contributing to the onset of additional Friedreich’s ataxia symptoms.
Diabetes
Diabetes, a condition that occurs when very high blood sugar levels are sustained over time, is seen in about 8%-10% of FA patients. Even more may have impaired glucose tolerance, where blood sugar is elevated but does not reach the threshold for diabetes.
Normally, a hormone called insulin that is produced in the pancreas helps glucose (sugar) in the bloodstream enter cells to be used as energy. But problems producing or responding to it can cause diabetes.
It’s believed that frataxin loss and subsequent deficiencies in cellular energy production can lead to the dysfunction and death of cells in the pancreas that secrete insulin. Moreover, energy deficiencies in fat and muscle cells can cause them to be unresponsive to insulin, called insulin resistance.
Symptoms of diabetes include:
- being very thirsty
- frequent urination
- weight loss
- fatigue
- blurry vision
- numb or tingling hands.
Bladder and bowel issues
Bladder and bowel problems in FA have not been thoroughly studied, but such symptoms have been reported in FA and found to negatively affect quality of life.
Some reported bladder and bowel problems in FA include:
- urinary frequency, which is the need to urinate many times throughout the day or night
- urinary urgency, or the sudden urge to urinate that may be difficult to control
- constipation
- urinary or fecal incontinence, involuntary urination or defecation.
Sexual dysfunction
Sexual dysfunction also may occur in FA, and has been found to be more likely in patients who also experience bladder or bowel symptoms.
Both male and female patients report sexual issues, including erectile dysfunction in men, insufficient vaginal lubrication in women, and reduced genital sensations in both sexes. Problems generally moving the body also may contribute to difficulties during sex.
How symptoms vary
While many symptoms can be observed in FA, their presence and severity is highly variable from patient to patient. Genetics may strongly influence which symptoms of FA a patient experiences and how fast they progress.
The most common type of mutation that causes FA is called a GAA trinucleotide repeat expansion, where a trio of DNA building blocks — GAA — is repeated too may times in a region of the FXN gene. The number of repeats in FA ranges from 66 to more than 1,000, whereas the normal number is about five to 33 in healthy people.
A greater number of repeats — which are associated with lower frataxin levels — is generally linked to earlier disease onset and more severe symptoms. More repeats have been linked to an earlier need for walking assistance devices and to heart disease.
FA age at onset is the other factor known to significantly affect disease presentation. While an FA diagnosis is most common before age 25, about a quarter of patients will develop the disease after age 25 (late-onset FA) or after age 40 (very late-onset FA). These forms of FA are associated with a slower disease progression than in typical FA. These patients may be less likely to develop certain symptoms, including cardiomyopathy or scoliosis, and may take longer to become wheelchair-bound.
Friedreich’s Ataxia News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Fatigue management relies on careful planning, being intentional
- LX2006 gene therapy now on FDA fast track for heart disease in FA
- How FARA brings together exercise, fundraising, and advocacy
- Managing reality, expectations, and hope with Friedreich’s ataxia
- FA advocate Kyle Bryant rides again for Team FARA and our community
Related articles

 Fact-checked by
Fact-checked by