Stem Cell-Derived Heart Cells Needed to Advance Understanding of Friedreich’s Ataxia Heart Disease
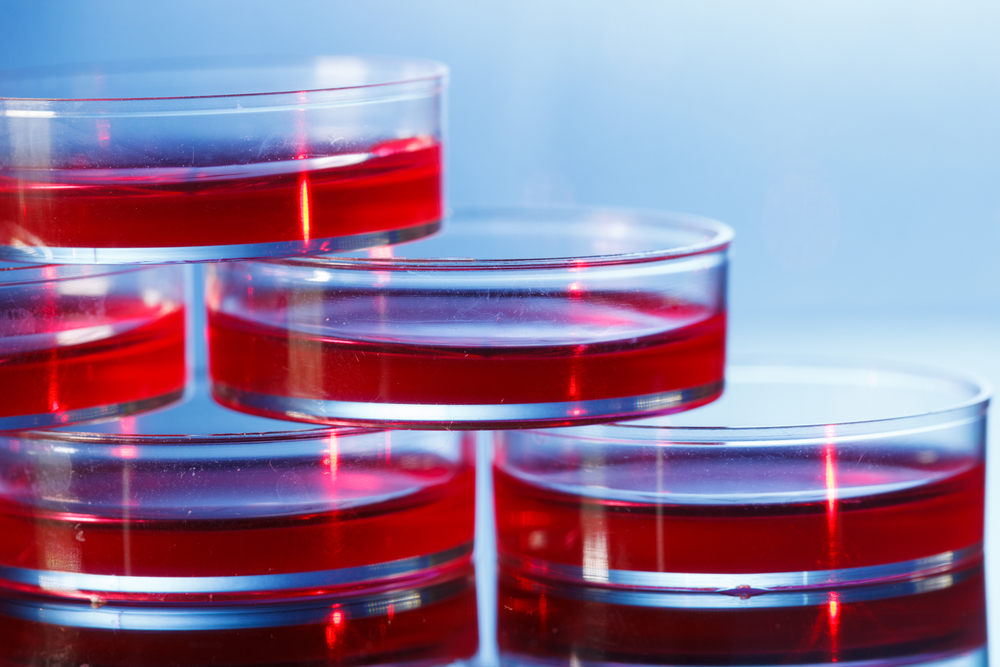
Heart cells grown from patient-derived, induced pluripotent stem cells can provide plenty of information about heart disease in Friedreich’s ataxia, a recent review argues, underscoring that such cell models are also the way forward to advance discovery of drug therapies.
However, the review, “Using human pluripotent stem cells to study Friedreich ataxia cardiomyopathy,” published in the International Journal of Cardiology, also highlighted that much work remains, to improve and validate the methods for discoveries of treatments.
Although heart disease is what kills most Friedreich’s ataxia patients, little is known about the cellular processes that cause heart abnormalities. Since animal models poorly capture the various aspects of the disease and its progression, scientists have used cell models to deepen their understanding of the disease processes.
Cells isolated from the skin and blood of patients are easily accessible, but as the disease mainly strikes in neurons and heart cells, the information such cells provide is limited.
With the advances in technologies allowing the production of stem cells from mature cells, isolated from patients, it has become possible to also study neurons and heart cells. But the methods still suffer limitations and drawbacks, researchers at the Royal Victorian Eye and Ear Hospital and the University of Melbourne, both in Australia, argue.
Heart cells grown from induced pluripotent stem cells have many of the characteristics of a real heart, contracting in a lab dish and having electrochemical properties that correspond to cells from different parts of the organ, including the ventricles and atria.
Research shows that such cells are immature, not really resembling an adult version. Nevertheless, studies of other genetic heart diseases using induced pluripotent stem cells show that immature cells also can model some aspects of adult disease.
The cells are studied most often as a single layer. To get information about how the cells work in a three-dimensional system, researchers need to grow so-called organoids — organ models grown in a lab dish.
Although induced pluripotent stem cells start to be explored in Friedreich’s ataxia research, few studies have focused on neurons or heart cells, the research team noted. Also, the studies that have been performed used only one or two cell clones from one or two patients.
Since individual cells might differ, studies are needed to analyze many cells from a larger number of patients to get reliable results, the authors recommended.
Finally, the team highlighted that studies need to show that a particular defect is reversed by elimination of the gene mutation, using gene-editing technologies.