Project on Potential Therapeutic Drug Targets in Spinocerebellar Ataxia Receives Funding
 The National Ataxia Foundation (NAF) recently awarded funding for 23 promising ataxia research projects. One of the projects is led by Dr. Ismael Al-Ramahi from Baylor College of Medicine in Houston, Texas and has received a “Pioneer SCA Translational Grant Award.” The project is entitled “Identification of druggable targets that modulate the levels of SCA-causing proteins in vivo” and focuses on finding gene targets whose modulation causes a reduction in the levels of the proteins responsible for spinocerebellar ataxia (SCA).
The National Ataxia Foundation (NAF) recently awarded funding for 23 promising ataxia research projects. One of the projects is led by Dr. Ismael Al-Ramahi from Baylor College of Medicine in Houston, Texas and has received a “Pioneer SCA Translational Grant Award.” The project is entitled “Identification of druggable targets that modulate the levels of SCA-causing proteins in vivo” and focuses on finding gene targets whose modulation causes a reduction in the levels of the proteins responsible for spinocerebellar ataxia (SCA).
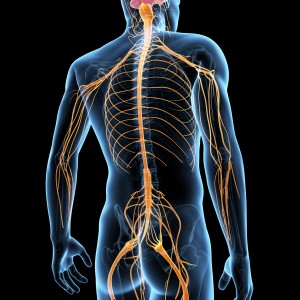
SCA is a progressive, neurodegenerative, genetic disorder that comprises several forms of disease (SCA1 to SCA29) and for which there is no cure or known effective treatment. It is characterized by a failure in muscle control and lack of balance and coordination due to the damage of parts of the nervous system that control movement.
This project is mainly focused on reducing the steady-state levels of proteins responsible for SCA, namely SCA1, SCA2 and SCA7. These SCAs correspond to polyglutamine diseases where a disease-associated protein (ataxin-1, ataxin-2 and ataxin-7, respectively) contains glutamine repeats (an amino acid referred to as “Q”) that exceed the normal stable threshold. “Six SCAs are caused by expansion of polyglutamine tracts leading to aberrant conformation and oligomerization, impaired degradation and increased accumulation of the corresponding proteins. With time, the polyQ-expanded proteins can trigger a variety of neuronal insults including transcriptional alterations, abnormal Ca2+ homeostasis, impaired vesicle transport, etc.” explained Dr. Al-Ramahi. The presence of these abnormal ataxin (ATXN) proteins ultimately results in neural damage.
Dr. Al-Ramahi hypothesized that a new therapeutic approach would be to reduce the levels of the proteins that lead to SCA. Previous studies in SCA1 animal models have shown that the decrease in mutant protein levels (by genetic manipulation) improved disease symptoms, even after the symptoms had already manifested in the animals.
“Based on this potential to not only delay but also reverse neurodegeneration, we set out to identify ‘druggable’ targets that modulate the levels of polyQ-expanded ATXN1, the SCA1-causing protein,” stated Dr. Al-Ramahi. Using genetic tools, human and Drosophila cell lines, and SCA1 mouse models, the team found that knocking down the expression of several components of the RAS–MAPK– MSK1 pathway reduced ATXN1 levels. The next goal of the team is to find additional “druggable” candidates that can also suppress ATXN1-induced neurodegeneration by modulating the protein levels.
It has been shown that SCA-causing proteins can be pathologically or functionally associated with each other, suggesting that druggable candidates eventually found for ATXN1 can also have a suppressing effect in other SCA proteins. The team will test the druggable candidate hits from the ATXN1 screen for their capacity to also reduce the protein levels of defective ATXN2 and ATXN7.
“The result of this project will be a number of drug gable targets with very high translational value for the treatment of SCAs,” concluded Dr. Al-Ramahi.






