Low Frataxin, Mitochondria Defects Prompt Cell Model Immune Response
Findings show new pathway that might contribute to FA disease mechanisms
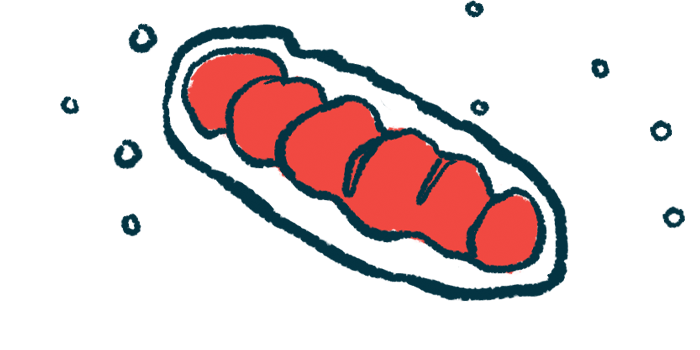
Low levels of the frataxin protein — the underlying cause of Friedreich’s ataxia (FA) — and the ensuing problems in mitochondria, the cells’ powerhouses, may activate certain immune responses in the disease, a study suggests.
In lab-grown human heart, muscle precursor, and connective tissue cells, suppressing frataxin production was linked to mitochondrial impairment, the release of mitochondrial DNA into the cytosol, and the activation of the type 1 interferon immune pathway. The cytosol is the liquid found inside cells that surrounds the nucleus (where all genetic information is stored) and other cellular organelles such as mitochondria.
Cells from FA patients also showed an excess of mitochondrial DNA in the cytosol and increased activity of a gene linked to activating interferon.
The findings overall “reveal a novel pathway that may contribute to the [disease mechanisms of FA] and that suggests points of therapeutic intervention,” the researchers wrote.
The study, “Activation of a type I interferon response associated with acute frataxin knockdown in iPSC-derived cardiomyocytes,” was published in Disease Models and Mechanisms.
FA is caused by mutations in the FXN gene that provides instructions for producing frataxin, a protein important for the proper function of the cellular organelles that produce energy, called mitochondria.
As a consequence of these mutations, not enough functional frataxin is produced and cellular energy production is disrupted. FA patients have damage to multiple systems, particularly in the nervous system and muscles.
Cardiomyopathy, a type of heart muscle damage that makes it harder to pump blood to the rest of the body, is also common and is “the leading cause of premature death” in FA patients, the researchers wrote. The mechanisms underlying cardiomyopathy in FA remain poorly understood, partially due to a lack of preclinical models that accurately mimic the condition.
Researchers in the U.S., mostly based in Philadelphia, developed a new cellular model to study FA-associated cardiomyopathy thereby bypassing the limitations of previously developed models.
Stem cells, which are able to become virtually any other cell type in the body under the right conditions, were obtained from healthy people and matured in the lab into cardiomyocytes, the heart’s muscle cells.
Effect on mitochondrial pathways
From this, the researchers developed two groups of cells: one wherein frataxin production was suppressed and another that was unmodified to use as controls. The two cell groups were the same except for frataxin levels.
Gene activity analyses of these lab-grown cardiomyocytes showed, as expected, that mitochondrial pathways were among the most affected in the low-frataxin group relative to controls.
Specifically, cardiomyocytes with low frataxin levels had severe mitochondrial impairment, with mitochondrial function genes having lower activity. When frataxin was reduced by about 50%, mitochondria was less able to respond to cellular energy demands.
The number of mitochondria was also decreased in low-frataxin cardiomyocytes, a finding that has been previously observed in heart tissue from FA patients and linked to cardiovascular disease.
The most affected pathway in low-frataxin cardiomyocytes compared with control cells was found to be in the activation of the type 1 interferon (IFN) pathway, which is part of the innate immune response, or the first line of defense, against viral infections.
When a molecule called IFN-beta is activated, it stimulates the production of proteins that prevent a virus from replicating.
A similar increase in type 1 IFN pathway was previously reported in a mouse model of FA and in fibroblasts, a type of connective tissue cell, derived from FA patients.
Recent evidence suggests that type 1 IFN responses can also be activated when mitochondrial DNA is released into the cytosol, which can happen under cellular stress. That DNA is recognized by a signaling pathway called cGAS-STING that triggers an immune reaction.
The activity levels of IFNB1, the gene coding for IFN-beta, were increased by about 170 times in cardiomyocytes with low frataxin levels compared with healthy cells.
In lab-grown human muscle precursor cells and fibroblasts, suppressing frataxin led to mitochondrial impairment, increased mitochondrial DNA in the cytosol, and higher activity of IFNB1 and interferon-stimulated genes. When the cGAS pathway was blocked, IFNB1 activity was reduced by 50%.
In lab-grown fibroblast derived from FA patients, mitochondrial DNA in the cytosol and activity levels of IFN1B and OAS-1 — a gene that codes for a protein stimulated by IFN-beta — were also higher compared with cells from healthy people. Blockade of the cGAS pathway significantly reduced OAS-1 activity levels.
These findings suggest that “decreased frataxin sensitizes mitochondria and makes them more prone to mtDNA [mitochondrial DNA] release,” the researchers wrote. “We observed mtDNA release into the cytosol following frataxin knockdown, as well as upregulation of IFNB1, mostly, although not entirely, through the activation of the cGAS-STING pathway. Taken together, these data suggest that release of mtDNA into the cytosol due to low frataxin can contribute to an innate immune response.”