Restoring Protein’s Levels May Correct Frataxin Deficiency and Mitochondrial Changes in FA, Study Suggests
Increasing the amount of a protein called GRP75 repairs the characteristic Friedreich’s ataxia (FA) frataxin deficiency and mitochondrial alterations, according to a study in patient-derived and mouse cells.
The study, “GRP75 overexpression rescues frataxin deficiency and mitochondrial phenotypes in Friedreich Ataxia cellular models,” was published in the journal Human Molecular Genetics.
FA is largely caused by GAA trinucleotide repeats in the FXN gene, with a small percentage of cases characterized by compound heterozygous mutations (two different mutated gene copies), with a point mutation — a change in only one nucleotide — in one gene copy, and an expanded GAA repeat in the other. Nucleotides are the building blocks of genes.
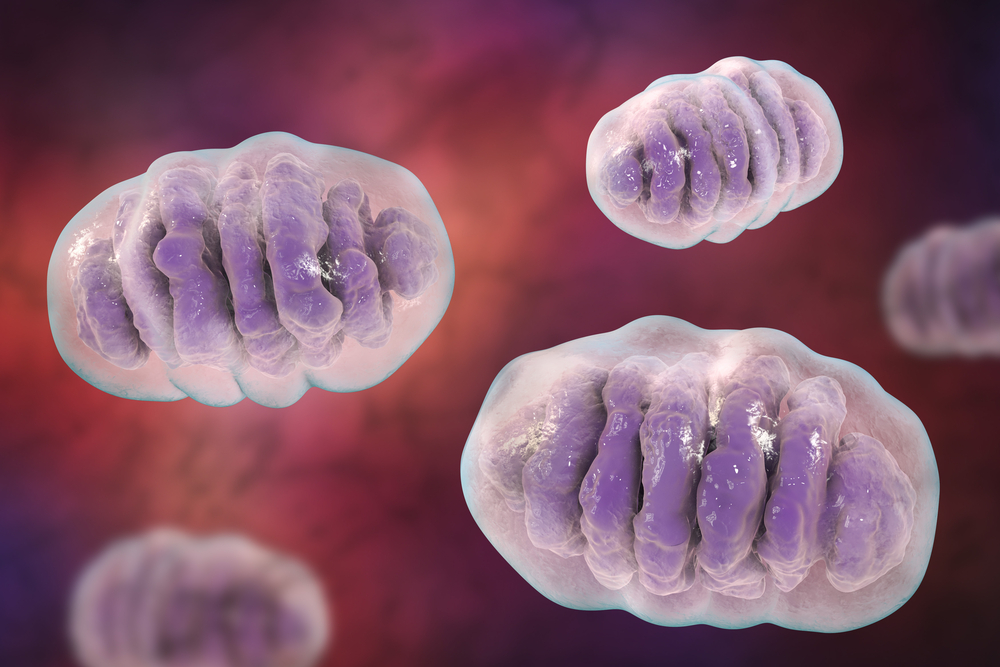
These alterations lead to lower levels of frataxin, an important protein for the proper functioning of mitochondria, the cell’s power plants. Frataxin deficiency lowers the activity of enzymes containing an iron-sulfur cluster, impairs mitochondrial function, and increases oxidative stress in these cellular organelles.
GRP75 is a protein with involvement in such functions as mitochondrial protein import and quality control, generation of iron-sulfur cluster-containing proteins, and mitochondrial homeostasis (stability).
GRP75 that fails to work as it should results in mitochondrial alterations, including abnormal structure and reduced production of ATP, the “molecular currency” of energy in cells.
If overproduced, GRP75 inhibits apoptosis — “programmed” cell death, as opposed to death caused by injury — and extends the lifespan of both human and nematode worm cells beyond their ideal, healthy span.
Previous studies suggested that GRP75 also affects the import, processing and maturation of frataxin. In vitro findings indicated that that these two proteins interact; in cancer cells, decreased GRP75 levels reduced the amount of frataxin.
Despite the data, scientists still do not know whether overproducing GRP75 reverses the functional defects of frataxin deficiency.
Aiming to address this issue, researchers at the Perelman School of Medicine at the University of Pennsylvania used cellular and molecular approaches to evaluate the interaction between GRP75 and frataxin in mouse neurons from the cerebral cortex.
Results revealed that abnormally high levels of GRP75 increase the levels of both wild-type (normal) and two clinically relevant frataxin mutations in cells. In contrast, exploring clinically meaningful GRP75 variants — including the Parkinson’s-associated mutations, R126W, A476T, and P509S — led to findings of impaired GRP75-frataxin binding and disrupted frataxin levels.
Importantly, GRP75 overproduction was able to repair both the mitochondrial fragmentation (fission) — seen with inhibitors of the mitochondrial energy production network — and the decreased ATP levels in skin fibroblasts and buccal cells (from the cheek) derived from FA patients. These patient-derived cells had originally shown lower levels of GRP75 and frataxin, “indicating that GRP75 reduction correlates with frataxin deficiency,” the researchers wrote.
The data suggested that the effect of GRP75 may be partially mediated by the interaction between GRP75 and the mitochondrial processing peptidase (MPP) — an enzyme complex that breaks up proteins — making frataxin more accessible to the MPP.
“As GRP75 levels are decreased in multiple cell types of [FA] patients, restoring GRP75 might be effective in treating both typical [FA] patients with two GAA repeat expansions and compound heterozygous patients with point mutations,” the scientists concluded.






