New experimental therapy targets rare FA mutation to restore frataxin
Variant has been reported in only three patients to date
Written by |
An experimental therapy may help increase the protein that’s missing or deficient in Friedreich’s ataxia (FA) in people with a rare mutation in the FXN gene, a new study suggests.
The therapy targets a rare mutation, known as c.165+5G>C, which has been reported in only three patients to date. The mutation leads to a problem called aberrant splicing, wherein a template molecule carrying genetic instructions from the FXN gene is abnormally processed, leading to a faulty frataxin protein being produced that has reduced function.
Using skin cells from a patient with this mutation, the study’s researchers showed that an experimental treatment called an antisense oligonucleotide (ASO) could help correct this processing. It led to more functional frataxin being produced in the lab, offering a potential path to treating FA in people with certain rare mutations.
The study, “Antisense oligonucleotide therapy for Friedreich’s ataxia patients carrying the c.165+5G>C splicing mutation,” was published in Molecular Therapy Nucleic Acids.
FA is a rare inherited disease caused by mutations in the FXN gene, which carries instructions for making frataxin, a protein that helps cells, especially muscle and nerve cells, produce energy. Without enough of it, nerve cells become damaged over time, leading to symptoms such as poor coordination, muscle weakness, and difficulty walking.
How does FA develop?
A person must inherit two faulty FXN genes — one from each parent — to develop FA. In about 96% of cases, both gene copies have a type of mutation called a GAA repeat expansion, where a short DNA segment is repeated too many times. In 4% of cases, one gene has a GAA repeat expansion and the other has a different kind of mutation. More than 60 mutations have been described, including several that are referred to as point mutations, where a single letter of the genetic code is changed.
That’s the case with the c.165+5G>C mutation, where the DNA building block guanine (G) is replaced by cytosine (C) in a certain location of the gene.
This change occurs in a section of FXN called an intron. Genes are made up of two types of segments — exons, which carry the actual instructions to make proteins, and introns, which are noncoding sections that are removed when the gene is read.
Normally, the cell stitches the exons together, in a process called splicing, to create a clean set of instructions for building a protein. But mutations in introns can disrupt this editing process, causing the cell to misread the gene. This leads to an abnormal protein.
ASOs are an emerging class of treatments that seek to restore normal splicing. By using small fragments of synthetic DNA that bind to the mutated site, they can ensure that introns are properly removed from the final molecule, allowing more functional frataxin to be produced.
“In the future, some recessive conditions may benefit from a ‘universal’ treatment, such as gene therapy or protein supplementation, while some will require individualized treatments that target a specific mutation,” the researchers wrote.
A new treatment combination
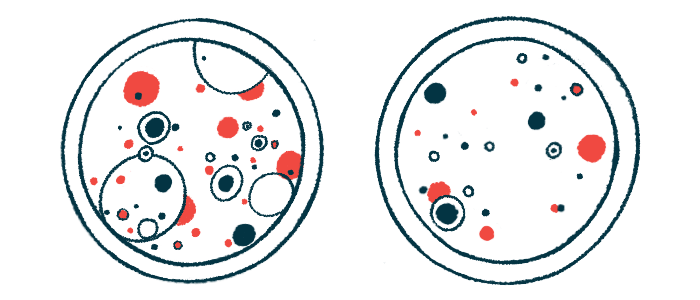
Here, researchers created several ASOs specifically designed to correct the splicing error caused by the c.165+5G>C mutation. They tested them in skin cells, or fibroblasts, from a person with this mutation on one FXN gene copy and a GAA expansion on the other.
Three of the ASOs increased the amount of FXN gene activity and protein levels by about two times, with the cells reaching about 50% of the protein levels seen in healthy cells.
The most promising candidate, ASO-82, was tested further. It worked only in cells with the c.165+5G>C mutation, confirming it was highly specific and didn’t affect cells with only GAA expansion mutations.
While ASO-82 boosted frataxin production, the levels still didn’t reach those in healthy cells, so researchers explored a combination approach where both mutations were targeted. Combining ASO-82 with another therapy that targeted GAA expansions resulted in a nearly 10 times increase in FXN gene activity — greater than the sum of each therapy’s individual impact.
“Patients carrying point mutations may benefit from combination therapy approaches that simultaneously target the point mutation-specific defect and general FXN insufficiency,” the researchers wrote.
More research is needed to understand the best way to deliver ASO therapies and to see if they’ll be safe and effective in clinical trials, but the findings represent a step toward developing treatments tailored to an individual’s specific genetic makeup.
“This ASO strategy may be therapeutically feasible for patients with [FA] with other point mutations that cause splicing defects,” the researchers wrote. “Success in developing treatments for disorders with only a few known cases will give hope to patients with [FA] carrying these rare point mutations.”