Statins Could Help Reduce Friedreich’s Ataxia Patients’ Risk of Heart Disease, Study Suggests
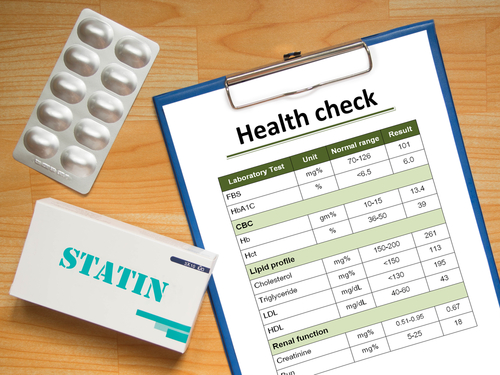
Statins, a cholesterol-lowering medication, can increase the amount of a good cholesterol component that is found in low levels in Friedreich’s ataxia patients, possibly helping them avoid heart failure, a Philadelphia study shows.
Scientists link poor levels of ApoA-I, as the good cholesterol protein is known, to an increased risk of heart disease — which, with heart failure, is a major cause of death among people with Friedreich’s ataxia. The research suggested that statins could help to protect against this.
The study, “Low apolipoprotein A-I levels in Friedreich’s ataxia and in frataxin-deficient cells: Implications for therapy,” was published in the journal PLOS One.
FA is a progressive disease whose hallmark is low levels of the mitochondrial protein frataxin. The disorder weakens limb muscles, but many patients experience heart muscle disease, or cardiomyopathy, which can progress to heart failure.
Scientists have linked lower levels of HDL, or good cholesterol, and its component, ApoA-I, to increased risk of heart disease and heart failure in the general population.
Research on the connection between HDL and ApoA-I levels and FA has generated conflicting findings. Some studies have reported lower levels of the substances in people with FA, but others have detected no differences between FA patients and controls.
Some scientists have said the conflicting results may reflect measurements of HDL and ApoA-I that are not sensitive enough.
Children’s Hospital of Philadelphia researchers decided to try an ApoA-I barometer they believed would be more sensitive. The method is called stable isotope dilution ultraperformance liquid chromatography-multiple reaction monitoring/mass spectrometry.
The team started by evaluating the levels of ApoA-I in blood collected from 95 FA patients and 95 healthy volunteers. Patients’ protein levels were 21.6% lower than the controls’.
“The 21.6% reduction in serum ApoA-I that we found in FA is very similar to the reduction levels (20.2%) that we found in tobacco smokers” — “another population at risk for heart failure,” the researchers wrote.
They found no correlation between FA patients’ ApoA-I levels and the length of GAA repeats in the DNA sequence of patients’ FXN gene. Shorter GAA repeats are the genetic cause of FA, scientists say.
To confirm that FA patients have lower ApoA-I levels, the team genetically engineered a human liver cell line, called HepG2, to generate less FXN activity. They put the fall-off at 70%.
The difference led to a 23% drop in ApoA-I production, the team said.
Next the researchers exposed the less active HepG2 liver cells to simvastatin, a drug commonly used to lower bad cholesterol levels while increasing ApoA-I levels.
Simvastatin significantly increased ApoA-I production in both less active FXN and the control cells. In fact, the two types of cells generated the same production, the researchers said.
The findings suggested “that statins could be used to increase serum ApoA-I levels in FA patients,” the team wrote.
They added that the experimental model they used showed that “there might be a threshold frataxin level where statins would not be effective.”
The researchers called for additional studies to better understand the correlation between the levels of frataxin the FXN gene produces and the levels of ApoA-I production.