Diazoxide-loaded droplets may be promising therapeutic approach
Blood pressure drug found to protect cells from oxidative stress-induced damage
Written by |
Diazoxide, a medication used to treat high blood pressure, protected cells — isolated from a person with Friedreich’s ataxia (FA) — against cellular damage caused by oxidative stress, suggesting it could be repurposed to treat the disease.
Because diazoxide can’t make it to the brain, which is affected by the nerve fiber damage and degeneration that characterize FA, researchers used tiny droplets made of fat to take diazoxide across the blood-brain barrier, a lining of tightly packed cells that keeps certain molecules, cells, and invaders from passing freely into the brain.
While the findings come from lab-grown cells, diazoxide may be a “potential therapeutic approach” for Friedreich’s ataxia, researchers wrote in the study “Microfluidic formulation of diazoxide-loaded solid lipid nanoparticles as a Novel approach for Friedreich’s ataxia treatment,” which was published in the Journal of Drug Delivery Science and Technology.
FA is caused by mutations that result in poorly functioning mitochondria, the bean-shaped structures that produce the energy cells need to survive. Nerve and muscle cells, which have high energy demands, become damaged, leading to FA symptoms.
Preclinical work found diazoxide may increase frataxin levels
Earlier preclinical work in Italy suggested diazoxide, which lowers blood pressure by widening blood vessels, may increase the levels of frataxin, the protein whose deficiency is a hallmark of FA, while reducing harmful oxidative stress in the brain.
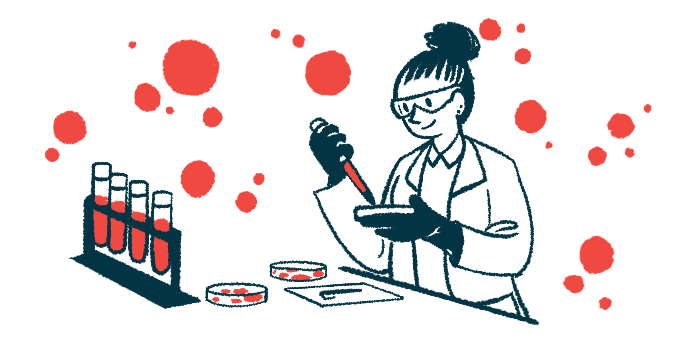
Now, the researchers developed tiny droplets made of fat, called lipid nanoparticles, as carriers to deliver diazoxine into brain cells. A so-called microfluidic device was used to prepare diazoxine-loaded nanoparticles that were consistent in size and formed no clusters.
In a lab model that mimicked the blood-brain barrier, diazoxine-loaded nanoparticles crossed it better than did diazoxine alone, suggesting that lipid nanoparticles may help deliver the medication into brain cells more effectively.
When added to fibroblasts isolated from a person with a diagnosis of Friedreich’s ataxia, diazoxine-loaded nanoparticles were readily uptaken. Fibroblasts are cells of the connective tissue that binds other tissues and organs in the body together.
Compared to diazoxine or nanoparticles alone, diazoxine-loaded nanoparticles significantly increase the proportion of fibroblasts that survived. Over time, these loaded nanoparticles also reduced the levels of reactive oxygen species, which cause oxidative stress.
The reduction in reactive oxygen species, which are a type of unstable molecules that are damaging to cells, was at least in part due to a reduction in the levels of reactive oxygen species produced by mitochondria. Poorly functioning mitochondria, such as those found in FA, usually produce excess reactive oxygen species.
While it is still early to know if these findings hold true in patients, they suggest diazoxine-loaded nanoparticles “as a promising and innovative formulation for safeguarding against oxidative stress induced damage,” the researchers concluded.