New Therapy SNH6 May Work for Cardiomyopathy in FA, Mouse Study Says
SNH6, a new dual-action therapy, has the potential to restore mitochondria function and may ultimately be used to treat cardiomyopathy in patients with Friedreich’s ataxia (FA), a mouse study found.
The compound’s dual mechanism allows it to both reduce the buildup of iron and modulate levels of important mitochondrial metabolites that are affected by the condition.
The study, “The Potential of the Novel NAD+ Supplementing Agent, SNH6, as a Therapeutic Strategy for the Treatment of Friedreich’s Ataxia,” was published in the journal Pharmacological Research.
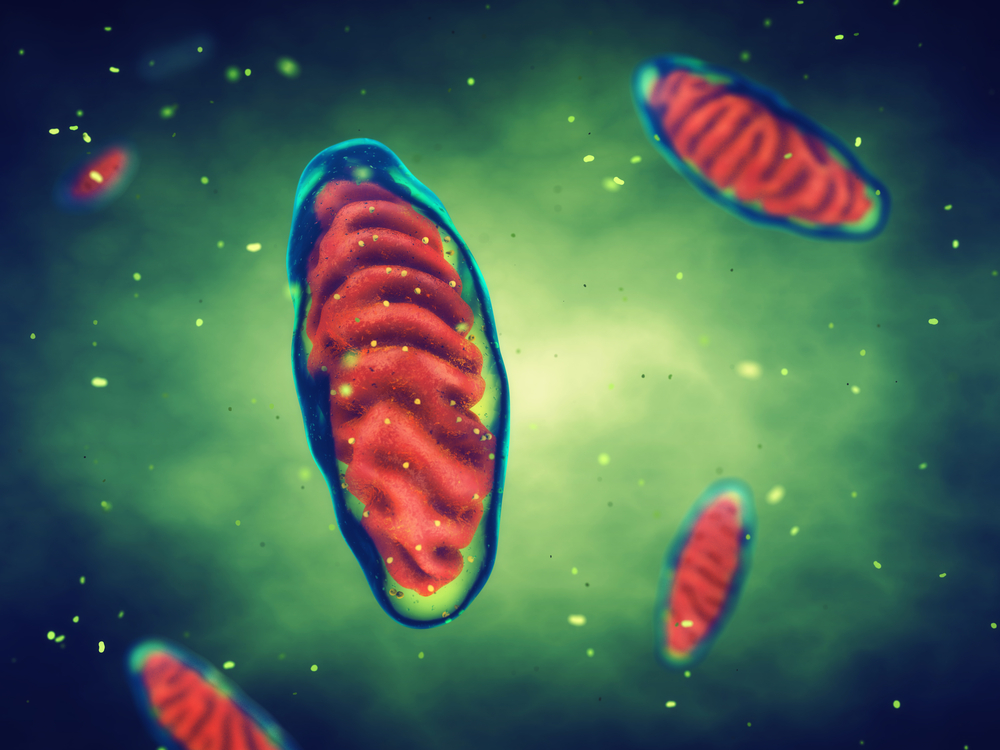
In people with FA, the lack of the protein frataxin triggers the buildup of iron inside mitochondria — the energy-producing structures within cells — resulting in the production of toxic reactive oxygen species that gradually damage mitochondria through a process called oxidative stress.
Damaged mitochondria become increasingly dysfunctional and unable to produce energy, eventually compromising nerve, muscle and organ function.
Nicotinamide adenine dinucleotide (NAD) is an essential metabolic co-factor involved in energy metabolism. Alterations to NAD metabolism, coupled with oxidative stress, and impaired energy production have been reported among those with FA.
New therapies that are able to restore mitochondria function by preventing iron accumulation and reversing alterations to NAD metabolism may be able to halt the progression of the disease.
Researchers at the University of Sydney and their colleagues designed SNH6, which acts both as an iron chelator and a vehicle to deliver a NAD precursor molecule directly to mitochondria.
An iron chelator is a molecule that is able to bind and scavenge iron, preventing its accumulation inside cells.
The NAD precursor is nicotinic acid, commonly known as niacin or vitamin B3. Once inside cells, SNH6 releases nicotinic acid, boosting the production of NAD, and it can also enter mitochondria to remove excess iron.
To test SNH6’s potential as a FA therapy, the team gave the compound to mice that had been genetically modified to be unable to produce frataxin. The animals had cardiomyopathy, a heart condition caused by the enlargement of heart muscles.
At the age of 4.5 weeks, mice with FA and healthy animals were randomly selected to receive either 20 mg/kg of oral SNH6, five days a week for four weeks, or a vehicle solution without SNH6 as a control treatment.
After reaching the age of 8.5 weeks, investigators sacrificed the animals to collect and examine their hearts, livers, and brains, and measure the levels of NAD, NAD metabolites, and other markers of mitochondria function.
They found significantly lower levels of NAD in the sick mice, regardless of treatment.
However, NAD levels in the hearts of treated mice, both those with and without FA, were significantly higher compared with untreated mice.
To find out why, the researchers measured the activity of enzymes in the cell nucleus (where a cell’s DNA is stored) that metabolize NAD and measured its consumption.
They found that NAD consumption was significantly higher in the hearts of mice with FA compared with healthy animals, which might explain why the basal levels of NAD were lower in sick animals.
Moreover, the activity of Sirt1 — an enzyme that relies on NAD to perform its function — was lower in mice with FA than in healthy animals. Similar alterations in NAD metabolism and Sirt1 activity were found in the brains and livers of sick mice.
Treatment with SNH6 raised the levels and the consumption of NAD, as well as the activity of Sirt1, in mice with FA. The researchers also found significantly higher amounts of the NAD metabolite nicotinamide (NAM) in the hearts of SNH6-treated FA mice, suggesting treatment increased NAD availability.
To evaluate the iron chelation abilities of SNH6, investigators used a cell-based test to measure iron release and uptake. At all concentrations tested, SNH6 triggered iron release and blocked its uptake in heart cells cultured in a lab dish.
A final examination of heart tissue for signs of cardiomyopathy found that, despite reducing the buildup of iron in the tissue, SNH6 failed to prevent the development of cardiomyopathy and to halt the progression of the disease.
“SNH6 is a novel therapeutic with significant pharmacological activity, which enhanced cardiac NAD+ and nuclear Sirt1 activity and decreased cardiac iron-loading in [FA] mice. No other agent yet designed for FA exhibits both these effective pharmacological properties,” the researchers said.
NAD+ is the oxidized form of NAD.
“Further studies are required to optimize the pharmacological properties of SNH6 to fully realize its therapeutic potential for the treatment of FA cardiomyopathy,” they said.