Copper Deficiency Found in Heart Tissue of Friedreich’s Ataxia Patients
Heart tissue from deceased patients with Friedreich’s ataxia was found to have quite low levels of copper, according to a recent study. Its authors suggest that copper supplements may benefit people with FA, although the link between copper levels and cardiomyopathy needs further research.
The study, “Abundance and Significance of Iron, Zinc, Copper, and Calcium in the Hearts of Patients With Friedreich Ataxia,” was published in The American Journal of Cardiology.
Cardiomyopathy (disease of the heart muscle) is a common cause of death in people with Friedreich’s ataxia, and is often accompanied by iron accumulating in cardiac muscle cells (cardiomyocytes). Other iron overload diseases, such as hemochromatosis and transfusion siderosis, show different iron distribution patterns, like a diffuse one in siderosis. Iron is a key contributor to cardiac cell death and inflammation.
Authors measured the levels of iron, but also levels of other metals — including zinc, copper, and calcium — in heart tissue taken during autopsies of people with Friedreich’s ataxia, in order to determine a potential correlation between the metal levels and the development of cardiomyopathy in FA.
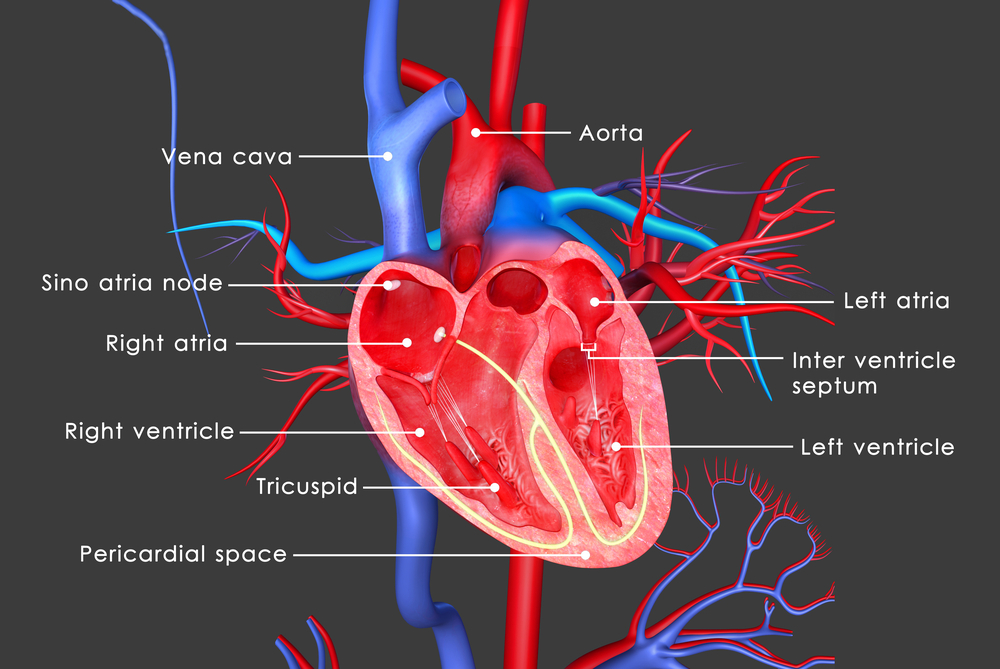
Researchers analyzed the metal in heart tissues (from both left and right ventricular walls) and the ventricular septum (wall separating the ventricles of the heart) of 23 Friedreich’s ataxia patients and eight controls (without the disease).
Total iron levels in the bulk heart tissue extracted from patients were not seen as elevated compared to controls. The same pattern was observed for zinc levels, which remained within normal ranges. Copper levels in the FA patient tissues, however, were significantly lower.
Whether low levels of copper contribute to the pathogenesis of Friedreich’s ataxia cardiomyopathy, or are a consequence of the heart disease, remains unknown. Authors suggest that clinicians should measure the copper levels in patients’ blood and, when low, prescribe copper supplements.






