Cardiac Pathology Explored in Friedreich’s Ataxia Patients

 A recent study published in the journal PLoS ONE characterized the association of the neurodegenerative disorder Friedreich’s ataxia with cardiac pathology. The study is entitled “The Pathogenesis of Cardiomyopathy in Friedreich Ataxia.”
A recent study published in the journal PLoS ONE characterized the association of the neurodegenerative disorder Friedreich’s ataxia with cardiac pathology. The study is entitled “The Pathogenesis of Cardiomyopathy in Friedreich Ataxia.”
Friedreich’s ataxia corresponds to a rare inherited disease characterized by progressive damage of the nervous system with degeneration of the spinal cord and peripheral nerves. This disorder is caused by a mutation in a gene called frataxin (FXN) that causes a reduction in the expression of the corresponding mitochondrial protein. Although Friedreich’s ataxia is best known for its disabling neurological features, the most common cause of death in patients is heart failure due to cardiomyopathy, a disease that affects the heart muscle (myocardium) making it weaker and less able to efficiently pump blood throughout the body.
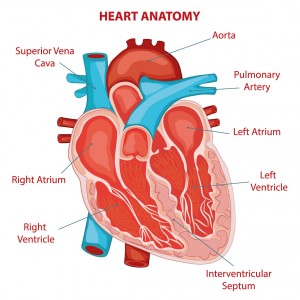
In this study, 28 archival autopsy tissue samples from hearts of patients with Friedreich’s ataxia and 10 tissue samples from healthy control hearts were analyzed to assess whether myocarditis (inflammation of the myocardium) is associated with the pathogenesis of Friedreich’s ataxia. Several measurements were performed including of the cardiomyocyte (cardiac muscle cell) hypertrophy, tissue frataxin assay, iron (Fe) histochemistry, X-ray fluorescence (XRF) of iron and zinc (Zn) in samples of right and left ventricular walls and interventricular septum, metal quantification in bulk digests by inductively-coupled plasma optical emission spectrometry (ICP-OES), and immunofluorescence and immunohistochemistry of cytosolic and mitochondrial ferritins and of the inflammatory markers hepcidin and CD68.
Researchers found that hearts from Friedreich’s ataxia patients exhibited hypertrophy, a reduced ventricular size and thickened walls. In addition, the cardiomyocytes were significantly larger than in control hearts and were surrounded by a fibrotic layer of connective tissue (also called endomysium).
The left ventricular wall had a severe reduction in cardiac frataxin levels. On the other hand, higher levels of iron were found in the left ventricular wall and ventricular septum in Friedreich’s ataxia patients, while the levels of zinc did not differ in comparison with the controls. Normal heart sections did not exhibit iron-rich inclusions, while in Friedreich’s ataxia hearts, small iron-positive granules were observed that assembled into aggregates in phagocytized cardiomyocytes. An abnormal number of CD68-reactive inflammatory cells was found in Friedreich’s ataxia hearts as well as cytosolic ferritin (a marker of excess iron) and hepcidin-containing cells. Hepcidin regulates iron levels and its failure to export the excess of iron from the immune cells is thought to be one of the causes of heart damage in Friedreich’s ataxia. The strong iron expression observed in the inflammatory infiltrate in cardiomyocytes might be unique for cardiomyopathy in Friedreich’s ataxia hearts.
The team concluded that myocarditis is an important mechanism in the pathogenesis of cardiomyopathy in Friedreich’s ataxia, and suggests that since the cardiac lesions observed occur in the presence of very low levels of frataxin protein, restoration of this mitochondrial protein and targeted anti-inflammatory therapy may be beneficial in patients with this disorder.






