New Evidence Shows Involvement of Glial Cells in Friedreich’s Ataxia
Written by |
Researchers have long known that — due to a genetic mutation — the levels of the protein frataxin are decreased in Friedreich’s ataxia. Because of the neurological nature of the disease, the effects of the mutation have mainly been studied in neurons within the central nervous system, and not much is known about the contribution of other cell types to the disease.
In an article, named “Frataxin knockdown in human astrocytes triggers cell death and the release of factors that cause neuronal toxicity,” Frida Loría and Javier Díaz-Nido at the Centro de Biología Molecular Severo Ochoa, the Universidad Autónoma de Madrid, and the Center for Biomedical Research on Rare Diseases (CIBERER) — all in Madrid, Spain – describe the results of their cell culture studies of frataxin in astrocytes. The study, published in the April 2015 issue of Elsevier journal Neurobiology of Disease, offers a new way of thinking around neuronal deficits in Friedreich’s ataxia.
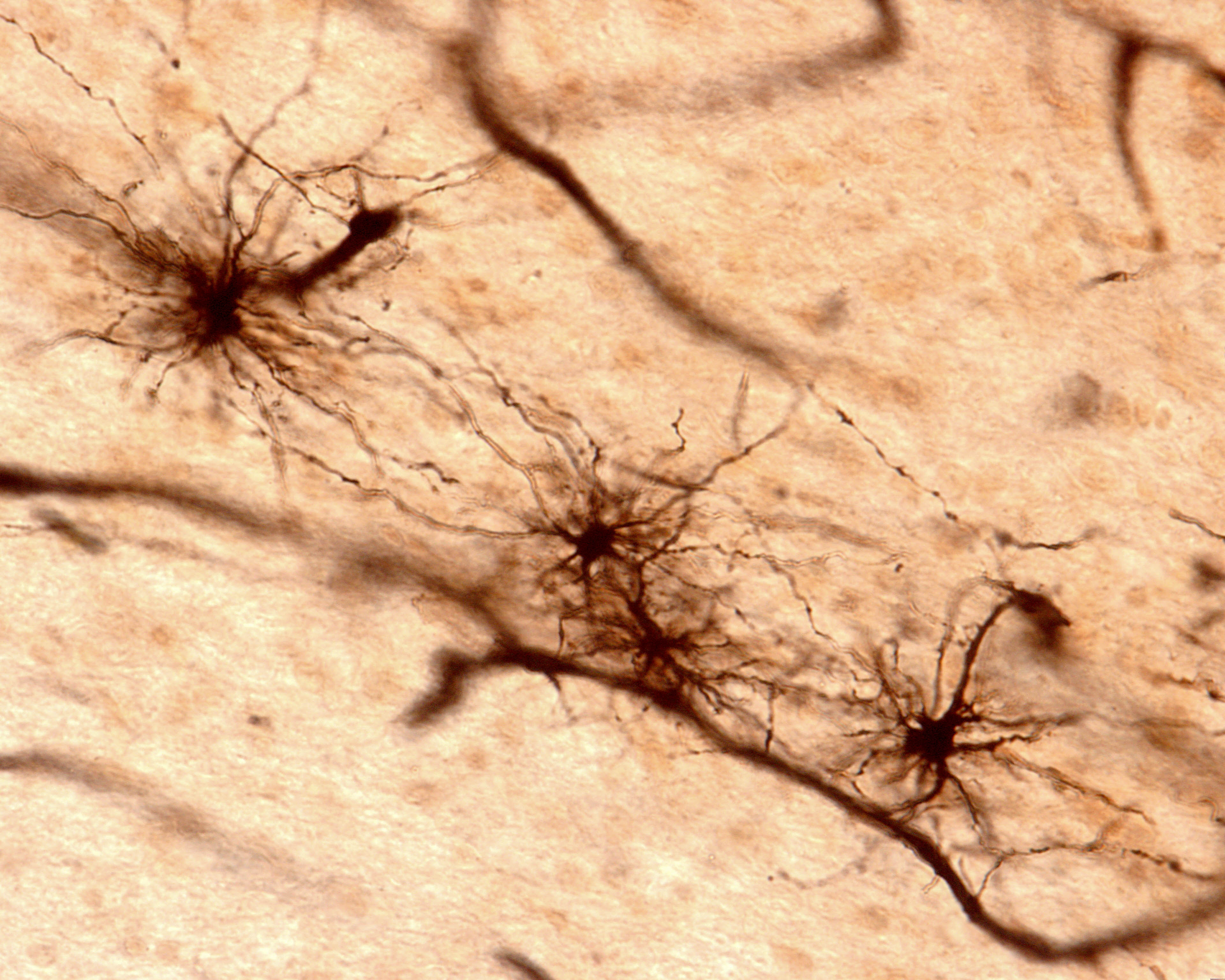
Astrocytes were for long considered to constitute only a supportive matrix for neurons, sometimes referred to as “brain glue.” Scientists now know that astrocytes — the most abundant glial cell type in the central nervous system — fulfill a large number of tasks in the brain and spinal cord. Astrocytes regulate blood flow and energy use, provide mechanical support, and protect neurons against oxidative damage. Most importantly, however, they have the ability to modulate the activity of neurons by releasing substances of their own, such as cytokines and growth factors. In analogy to the term neurotransmission, the term gliotransmission has now generally been adapted to describe the modulatory signaling by glial cells.
By knocking down the gene coding for frataxin in cultured human astrocytes, the team managed to reduce the gene and protein expression in cells to a level similar to what is found in patients: 10 percent to 25 percent of normal values.
Frataxin is a protein found in cell’s mitochondria, which are cellular energy producers. The study found that apart from having an abnormal shape in the astrocytes lacking frataxin, the mitochondria produced higher levels of superoxide — an oxidant toxic to neurons.
In accordance with this finding, researchers observed that cell survival and total number decreased following knock-down of frataxin in astrocytes. The team believes this finding is linked to the increased activity of p53, p21 and activated caspase-3, a molecular trio usually involved in apoptosis (programmed cell death).
Considering that astrocytes are an important source of inflammatory cytokines, growth factors, and other signaling molecules in the brain, the team also decided to take a look at the substances secreted by the cells into the culture medium. As suspected, astrocytes lacking frataxin displayed abnormal secretion of 55 different molecules, mainly associated with cell growth, immunity, and inflammation. Such a highly altered profile of secreted signaling factors is likely to have a profound effect on neurons. To test this hypothesis, scientists then cultured mouse neurons in medium collected from the deficient astrocyte cultures. The neurons, grown in the molecular environment of frataxin lacking astrocytes, did not develop normally, showing a 50 percent decrease in the branching of cell processes (axons and dendrites) as well as in neuronal density.
The study confirms that frataxin is crucial not only for neurons but also for the normal function of astroglia. It is an important reminder to the research community to study cell types other than neurons in Friedreich’s ataxia. More importantly, however, it points to the necessity to further investigate interactions between neurons and glial cells to better understand neurological diseases such as Friedreich’s ataxia.





