In Friedreich’s Ataxia, Frataxin Protein Levels May Determine Nature of Disease
Written by |
A recent study links frataxin protein levels to disease features in patients with Friedreich’s ataxia (FA). The article, titled “Frataxin levels in peripheral tissue in Friedreich ataxia,” was published in Annals of Clinical and Translational Neurology journal.
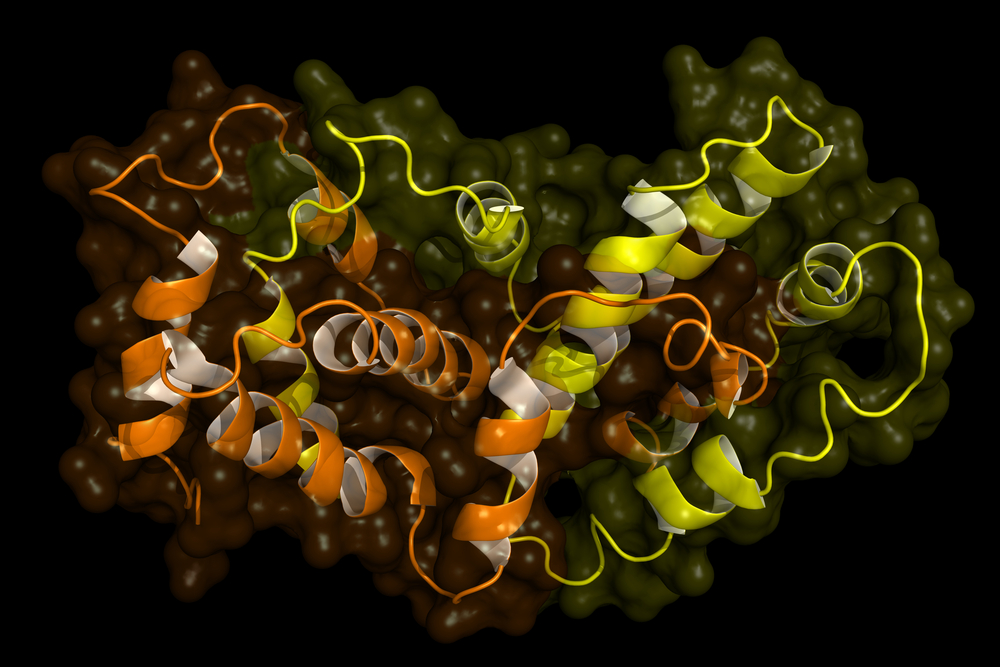
FA is a neurological disorder that progressively damages the nervous system, resulting from a mutation in a gene called frataxin (FXN). In 98% of affected individuals, the mutation expands the sequence of nucleotides’ building blocks (guanine–adenine–adenine, or GAA) repeats in FXN.
Researchers explored the relationship between frataxin protein levels and disease features. A total of 521 FA patients with no significant differences in mean age or sex, of which 306 were carriers and 120 served as controls, were considered for this study. Blood and buccal cell samples were extracted from the subjects at clinical visits. Additionally, the team injected the mutant frataxin gene into human kidney cells to create mutations within the cells.
The results suggested no evidence of increased levels of frataxin protein over time, although a small increase was detected over decades by means of linear regression analysis. In both affected and unaffected tissues, number of GAA repeats were linked to levels of expressed frataxin protein that, in turn, were associated with age. Patients with lower numbers of GAA repeats had reduced levels of frataxin when compared to patients with higher GAA repeats. Importantly, levels of frataxin protein were linked to mutation types, with some reducing frataxin levels and others maintaining regular levels of the protein, either in vitro, in vivo or both.
These findings highlight the link between frataxin protein levels and disease characteristics in FA patients. However, multiple mechanisms may contribute to the elevated levels of frataxin in the blood of some patients. “Thus, the present work demonstrates the complexity of peripheral frataxin levels in FA, and the need for consideration of multiple factors in interpretation of the results of clinical intervention studies,” the authors conclude.