MRI detects brain changes in early Friedreich’s ataxia
Patients had significantly reduced volumes in areas of the brain, brainstem
Written by |

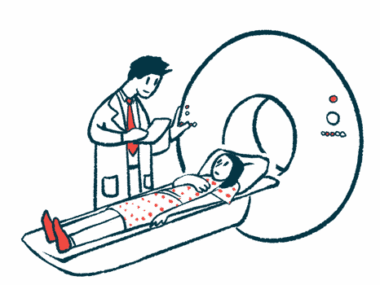
MRI scans detect large- and small-scale changes in various areas of the brain and brainstem in the early stages of Friedreich’s ataxia (FA) over time, a new study reports.
Many of the changes occurred outside the cerebellum, a brain region primarily implicated in the motor problems associated with FA.
The MRI measures may therefore be useful as new biomarkers of disease progression for clinical trials, the researchers noted in “Brain MRI detects early-stage alterations and disease progression in Friedreich ataxia,” which was published in Brain Communications.
FA is an inherited, progressive disorder that mainly affects the nerves and the muscles they control. MRI scans of FA patients show wasting in certain areas of the nervous system, including the brain stem and cerebellum, the structure at the back of the brain primarily responsible for balance and movement.
Studies of detailed changes in brain structure, and those that occur over time, are limited, however, especially for early stage FA.
MRI differences in Friedreich’s ataxia
Researchers at the University of Minnesota enrolled 28 people (50% female) in the early stages of FA, with a mean age of 19. A group of 20 age- and sex-matched unaffected people served as controls. Clinical and imaging data were collected at the start of the study (baseline) and after one, two, and three years.
Clinical data included the Friedreich Ataxia Rating Scale (FARS), the Scale for the Assessment and Rating of Ataxia (SARA), functional stage, activities of daily living, and the 9-hole peg test to assess the function of the nondominant hand.
Initial MRI imaging showed the FA patients had significantly reduced volumes (wasting) in various areas of the brain and brainstem over the controls. They included the medulla in the brainstem, the midbrain at the top of the brainstem, and the pons between the medulla and midbrain.
The white matter (nerve fibers) of the cerebellum, the white matter tracts that connect the cerebellum to the midbrain — called the superior cerebellar peduncles — and the thalamus in front of the midbrain were also significantly smaller.
Over time, there was a 1% loss of the total white matter of the cerebellum per year. There was also a 0.7% loss of the total cerebellum volume, as well as the cerebellar gray matter volume (nerve cell bodies), both of which were similar to the controls at baseline. There was also a 0.7% loss per year in the pons and midbrain, and a 1.9% loss per year of the thalamus.
The largest change was seen in the fourth ventricle, a cavity between the brainstem and cerebellum, with an increase in volume of 3.9% per year.
Diffusion tensor imaging was used to examine small-scale structural (microstructural) brain and brainstem changes associated with FA. This MRI technique tracks water flow patterns within the brain, which can reveal microscopic details about tissue architecture.
Compared with the controls, people with FA had increased water flow in many areas of white matter, a sign of reduced white matter integrity due to nerve fiber damage.
The most considerable difference was in the white matter tracts of the superior cerebellar peduncles (cerebellum to midbrain), followed by the inferior cerebellar peduncles, which connect the spinal cord and medulla to the cerebellum. These two white matter structures also showed signs of worsening damage, as indicated by increasing water flow values over time.
FA patients had significantly reduced nerve fiber density and a lower cross-sectional area of the nerve fiber bundles in both cerebellar peduncles, as well as the corticospinal tract, a whole brain analysis showed. This primary pathway connects the spinal cord to the brain to enable movement.
None of the MRI measures related to the cerebellum correlated with clinical assessments, a surprising result, according to researchers.
A higher volume of the fourth ventricle and the cerebrospinal fluid, which surrounds the brain and spinal cord and fills the ventricles, strongly correlated with worse scores across all clinical measures. A lower thalamus volume was associated with worse scores for FARS, SARA, and functional staging.
Changes in water flow parameters in the superior cerebellar peduncles also strongly correlated with all clinical scales, except for FARS.
“Our study shows that several MR metrics are sensitive to disease progression in the brain,” the researchers said. “These MR metrics may therefore constitute useful novel biomarkers of disease progression for clinical trials.”