Synthetic SS-31 Peptide Could Be Used to Treat Friedreich’s Ataxia, Study Reports
The synthetic peptide SS-31 increased production of the frataxin protein that is missing in Friedreich’s ataxia, a Chinese study reports.
Researchers said the finding raises the possibility that scientists could develop an FA therapy around SS-31. Peptides occur naturally as components of proteins.
The team published its study in the journal Nature Scientific Reports. The title is “Peptide SS-31 upregulates frataxin expression and improves the quality of mitochondria: implications in the treatment of Friedreich ataxia.”
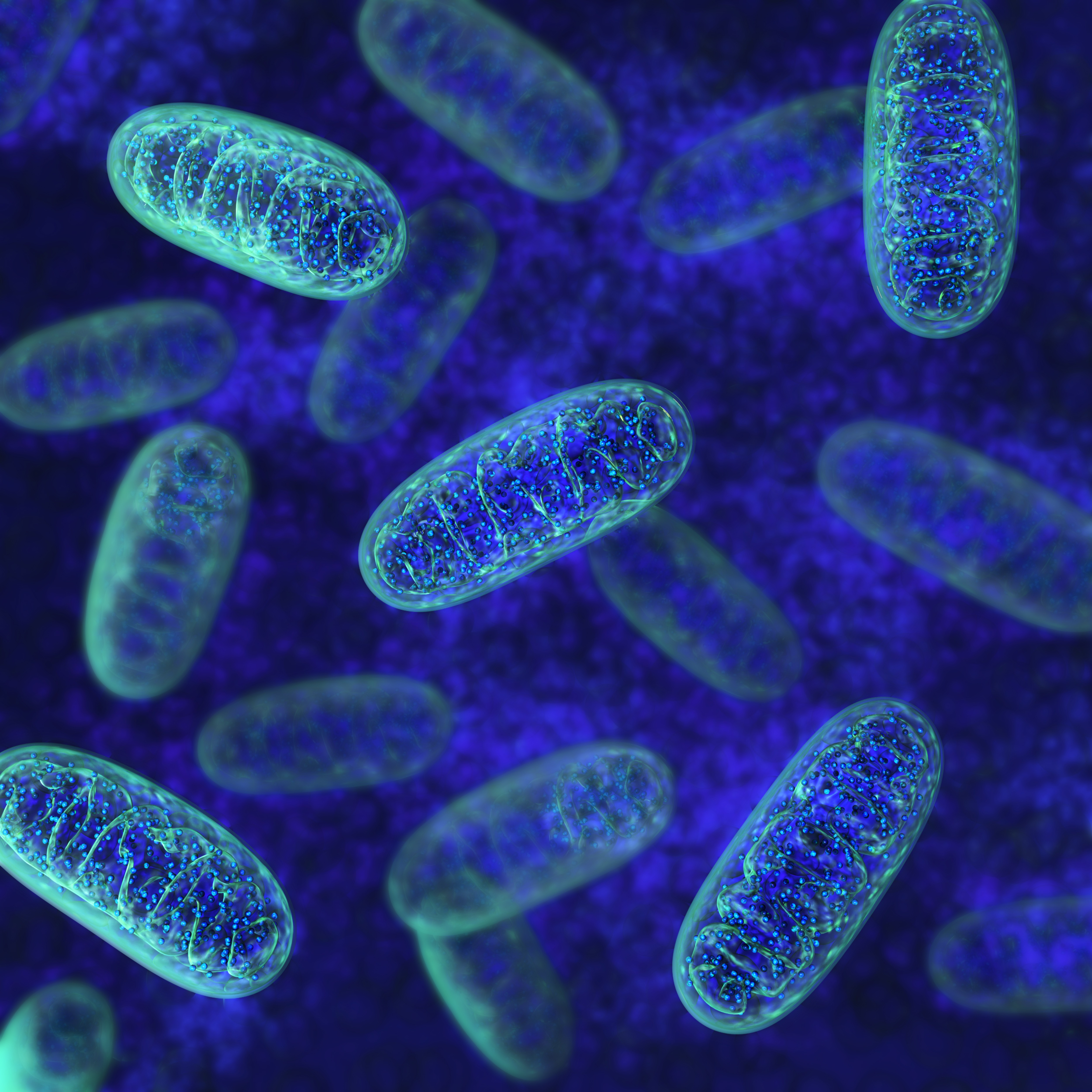
Scientists have determined that the cause of FA is lack of frataxin. The protein is crucial to the functioning of mitochondria, or cell components that generate energy. Lack of frataxin damages nerve cells, the heart and other organs.
When frataxin levels are adequate, they decrease the formation of reactive oxygen species, or free radicals. Free radicals can harm mitochondria by causing oxidative stress — an imbalance between the body’s production of free radicals and its ability to counteract their harmful effects.
Lack of frataxin leads to a surge in free radicals, damaging mitochondria and ultimately killing nerve cells.
At one point, researchers looked at whether antioxidants such as MitoQ or idebenone could treat FA by reducing oxidative stress. Their efforts failed, however.
Researchers are now working on a number of new approaches to treating the disease.
SS-31, short for Szeto-Schiller 31, is a peptide whose natural form in found in the inner membrane of mitochondria, an area where free radicals are produced. Animals studies have shown that SS-31 reduces free radical production and decreases oxidative stress, improving diseases stemming from mitochondria dysfunction.
Researchers at the Medical School of Nanjing University decided to see how SS-31 would affect cells known as lymphoblasts and fibroblasts that were taken from FA patients. A lymphoblast develops into a white-blood-cell component of the immune system known as a lymphocyte. A fibroblast develops into connective tissue.
When scientists study FA, they prefer to work with neurons or heart muscle cells known as cardiomyocytes. They are hard to study in a laboratory, however. Because lymphoblasts have low levels of frataxin, scientists often study them instead.
The Chinese researchers discovered that SS-31 lowered frataxin-deficiency-triggered oxidative stress in lymphoblasts and fibroblasts. Interestingly, SS-31 increased frataxin levels in a dose-dependent manner, meaning that the higher the dose, the more protein produced. This suggested that SS-31 could be a way to treat frataxin deficiency and thus FA itself.
In addition, the researchers discovered that SS-31 bolstered mitochondria’s ability to ward off damage from oxidative stress.
The team said studies are needed to determine how SS-31 increases frataxin production. But “improvement in the quality of mitochondria in FRDA [Friedreich’s ataxia] patient–derived cells by SS-31 treatment appears promising,” they said. “It is reasonable to suggest that SS-31 might potentially be a new drug for the early treatment” of FA, they concluded.






