Stem Cell-secreted Molecules Restore Function to Human Friedreich’s Ataxia Cells
Molecules released by certain stem cells may promote an increase of frataxin protein and rescue cellular function, researchers have shown in a cell model of Friedreich’s ataxia.
The study, “Mesenchymal Stem Cell-Derived Factors Restore Function to Human Frataxin-Deficient Cells,” was published in the journal The Cerebellum.
Friedreich’s ataxia is a genetic neurological disorder characterized by mitochondrial dysfunction due to a deficiency of frataxin protein. This protein is important for the proper maintenance and protection of neurons. There is no cure for the disease, but potential therapies include drugs that improve mitochondrial function and reduce oxidative stress (a detrimental consequence of mitochondria dysfunction).
Stem cells, particularly those known as mesenchymal stem cells (MSCs), are being investigated extensively as potential treatments for a wide range of diseases, including neurological disorders. Their potential neuroprotective effect is linked to the secretion of several factors that may benefit neuronal health via anti-oxidant actions.
“If stem cell therapies are to become a viable therapeutic approach for central nervous system (CNS) degeneration, a precise understanding of their effects on neurons is required,” researchers wrote.
Join our FA forums: an online community especially for patients with Friedreich’s Ataxia.
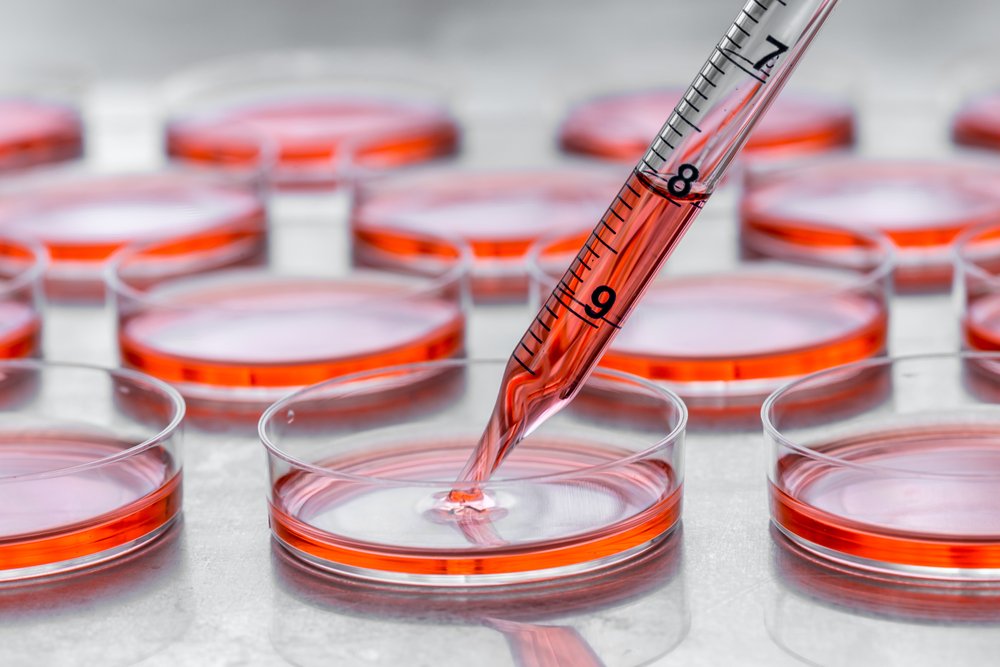
They developed a cellular model of frataxin deficiency by reducing frataxin expression in a neuroblastoma cell line, SH-SY5Y, widely used in neurological studies. As is observed in Friedreich’s ataxia patients, the reduced frataxin expression led to decreased cellular viability and defective anti-oxidant responses.
When the frataxin deficient cells were exposed to MSC conditioned medium (where the MSCs grew), the cells increased the levels of frataxin protein. And exposure to MSC conditioned medium also led to increased expression of molecules associated with frataxin’s anti-oxidant functions, including PGC1a, Nrf2, superoxide dismuting enzymes (SOD 1 and 2), and the enzyme catalase.
“The increase in catalase induced by MSC conditioned medium is of relevance, since hydrogen peroxide scavenging has been shown to rescue frataxin deficiency in a [Friedreich’s ataxia] Drosophila model,” researchers wrote.
Researchers looked also to the effects of low frataxin on cellular proliferation and differentiation, and found that a particular cell type, Schwann cells, showed reduced expansion and formation. These cells produce the myelin sheath around neuronal axons and may also be defective in Friedreich’s ataxia patients.
While frataxin-deficient SH-SY5Y cells showed an inability to differentiate to Schwann cells, exposure to MSC conditioned medium stimulated the differentiation.
Overall, “we show MSC-secreted factors were able to protect against the cellular dysregulation induced by frataxin deficiency. The demonstration that factors produced by MSCs can regulate frataxin expression and restore cellular homeostasis suggests that they may have potential therapeutic benefits for patients with Friedreich’s ataxia,” according to researchers.