IFN-γ-1b Helps 12 Friedreich’s Ataxia Patients in Trial
 Results are in for an open-label phase 2 clinical trial of interferon gamma (IFN-γ) treatment for Friedreich’s ataxia (FRDA) sponsored by Children’s Hospital of Philadelphia along with collaborators at the Friedreich’s Ataxia Research Alliance and Vidara Therapeutics Research Ltd. David Lynch, MD, PhD, served as the principal investigator. The trial, “Interferon Gamma-1b in FRDA,” was initiated in August 2013, and results were updated in October 2014.
Results are in for an open-label phase 2 clinical trial of interferon gamma (IFN-γ) treatment for Friedreich’s ataxia (FRDA) sponsored by Children’s Hospital of Philadelphia along with collaborators at the Friedreich’s Ataxia Research Alliance and Vidara Therapeutics Research Ltd. David Lynch, MD, PhD, served as the principal investigator. The trial, “Interferon Gamma-1b in FRDA,” was initiated in August 2013, and results were updated in October 2014.
According to the article, “Open-label Pilot Study of Interferon Gamma-1b in Friedreich Ataxia,” IFN-γ on-average improved Friedreich Ataxia Rading Scale (FARS) scores in 12 patients with FRDA. However, it is unclear the mechanism by which treatment helped the patients.
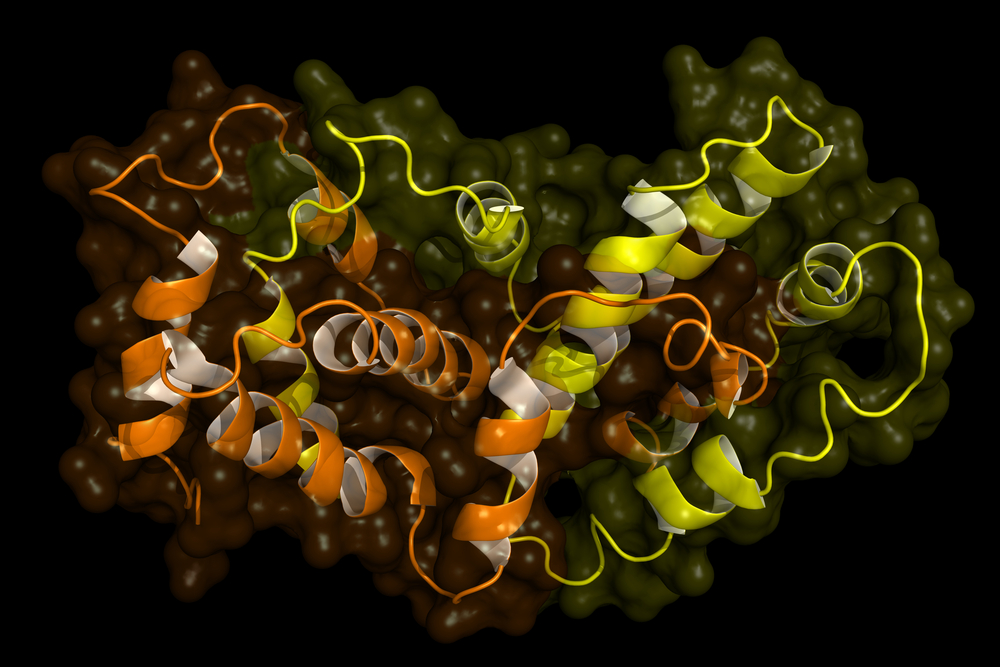
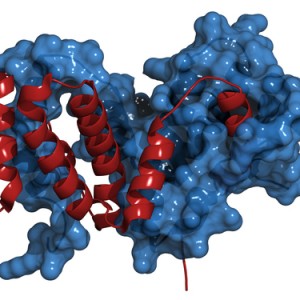
The trial was initiated due to a previous study that reported an increase in frataxin protein levels in response to IFN-γ. This may not have been the case in the present study, as “no statistically significant relationships were observed between frataxin protein levels, FARS scores, and in vivo IFN-γ levels,” wrote the authors.
Frataxin level in whole blood was the primary outcome of the trial. The 12 enrolled patients, all between the ages of 5 and 17 years, received subcutaneously injected IFN-γ thrice weekly for 12 weeks. Initial dosing was 10 mcg/m2 for two weeks before it was increased to 25 mcg/m2 for another two weeks; after, the dose was increased to and remained at 50 mcg/m2 (the FDA-approved dose for children) for the last eight weeks of the study. In addition to whole blood frataxin levels, frataxin levels in multiple other tissues were measured, as well as frataxin mRNA. Finally, FARS scores and other neurologic evaluations were used as additional secondary outcome measures.
Throughout the study, patients tolerated IFN-γ without serious adverse events. Only two patients reported a severe adverse event, and their IFN-γ doses were reduced.
In conclusion, the authors believe that “larger, longer placebo-controlled trials including biochemical assessments in affected tissues are necessary to evaluate fully the efficacy and utility of IFN-γ in FRDA.” Until then, the team may continue to develop its IFN-γ therapy, trademark name of “Actimmune,” to treat patients with FRDA.